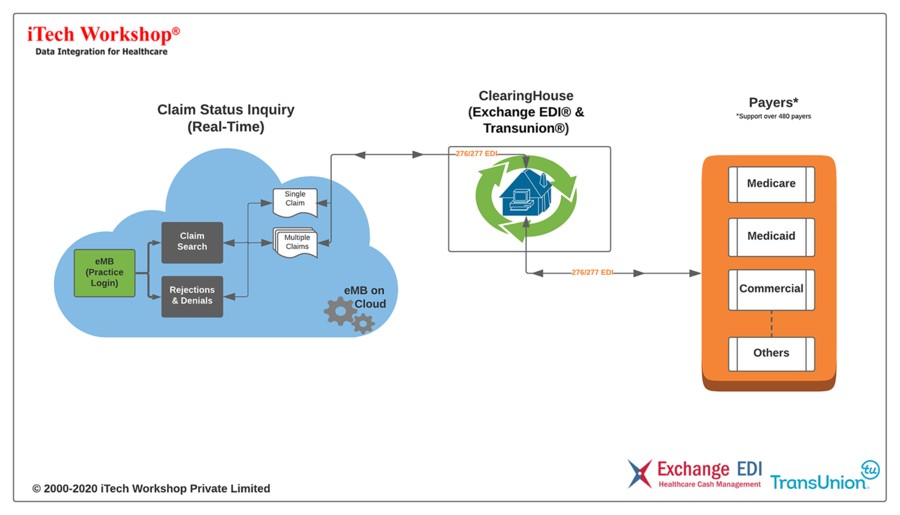
iTech has introduced a “Seamless Claim Status Inquiry” feature in its expEDIum Medical Billing (eMB) product to make seamless inquiries from the original claims submitted through eMB.
BANGALORE, INDIA, December 08, 2020 /Neptune100/ — iTech, a Healthcare IT Solutions vendor specializing in delivering a secure, affordable, and comprehensive Web-based Medical Billing & Practice Management Solution, implemented a seamless claim status inquiry to their expEDIum product suite.
CAQH® 2019 Index states that “Medical plan adoption of electronic claim submissions is at 96 percent, adoption of claim status inquiry is at 70 percent & adoption of eligibility and benefit verification is at 84%.” To handle aged and denied claims, billers must know the claims’ status by making AR calls to various payers which is time-consuming and expensive for the clinics. Now in expEDIum, the new claim status inquiry feature creates a seamless process to pull several aged, denied claims, initiate inquiries, and use the system to follow up on such claims effectively thus saving accounts receivables cost. expEDIum already supports seamless Insurance Eligibility Verifications (IEV). expEDIum Product suite does not support prior authorization as the industry adoption of standardized, electronic Prior authorization remains low relative to other HIPAA mandated electronic transactions.
There is a per-transaction fee that applies to both Claim Status Inquiries and Insurance Eligibility Verifications when performed from expEDIum suite of products.
iTech currently uses Exchange EDI® as our preferred clearinghouse for Claim Status Inquiries and Insurance Eligibility Verifications.
About Exchange EDI
Exchange EDI is a leader in the Healthcare Network connecting providers, payers, and patients with healthcare EDI needs such as Eligibility, Claim Status, Estimation, and Prior Authorization on one integrated platform. Exchange EDI enables providers to get paid more efficiently at a lower cost with fewer incidents of fraud, and users and patients to experience a simple, convenient way to the data. The Exchange EDI Network process over several million transactions annually for healthcare users that expands across the United States. Visit Exchange EDI on the web at www.exchangeedi.com
About iTech Workshop:
iTech, a Healthcare IT Solutions vendor specializing in delivering a secure, affordable, cloud-based, scalable Practice Management Software, Medical Billing, Electronic Claims Processing, and RCM solutions. iTech’s expEDIum Suite are serving specialties such as Behavioural, Public Health, Gastroenterology (GI), Podiatry, Ambulance/EMS & Cardiology. The expEDIum Suite of products consists of expEDIum Medical Billing, expEDIum Claims Portal, expEDIum Pay & expEDIum Reports. We currently have over 2000 providers, over 200 clinics on the system, processing about 1.2 million HCFA & UB04 claims and about 5 million HIPAA transactions per year. Currently, around 100 public health clinics (100 counties in over 20 states) use the system through our EMR partner.
Siva Narayanaswamy, Executive Director & CEO
Email: [email protected]
Phone: 786-646-0099 Ext 1001
www.itechws.com,www.expediumrcm.com